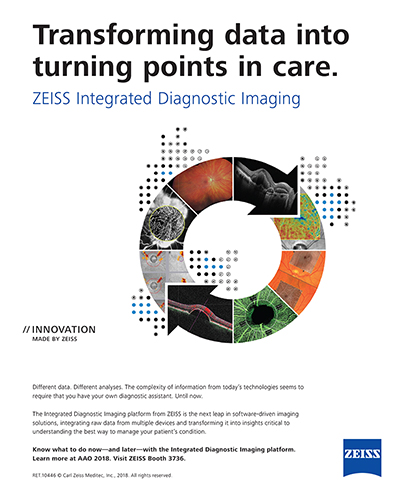
Figure 1. Fundus photography performed by the patient’s referring optometrist showed areas of hemorrhage and microaneurysms (A), while neovascularization was evident on widefield imaging (B).
- A case of a 49-year-old African-American man with a 7-year history of diabetes.
- At the time of the evaluation, his hemoglobin A1C level was 8.9, and historically, it had been around 8 to 9 since diagnosis.
- The IOP was 21 mm Hg in each eye.
- A fundus photograph obtained during a previous visit with an optometrist showed areas of hemorrhage and microaneurysms for 360° (Figure 1A).
- Hemorrhage was evident in four quadrants in each eye.
- Areas of neovascularization were evident on ultrawide-field imaging (Figure 1B).
Treatment Plan
- The optometrist recommended follow-up 6 months later.
- The patient returned in 6 weeks with decreased vision and pain in both eyes.
- At that time, VA was 20/20 OU, and IOP was 43 mm Hg OD and 35 mm Hg OS.
- The patient was referred to me and was seen on the same day.
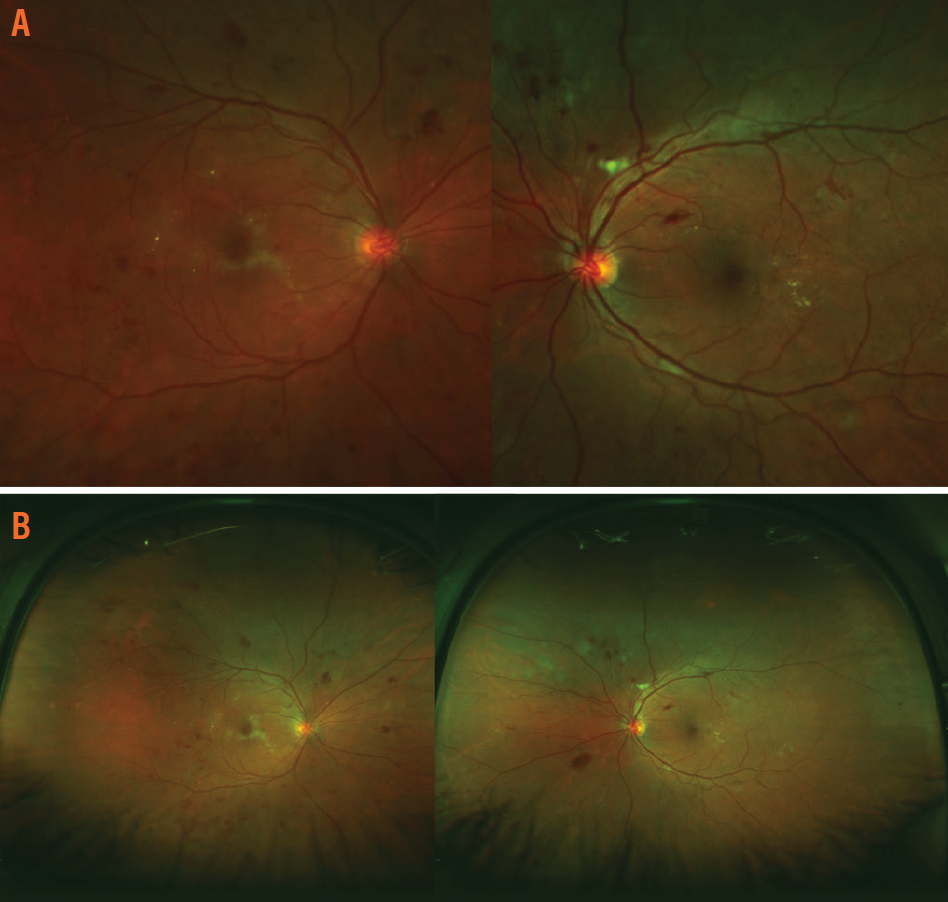
- A fluorescein angiogram showed nonperfusion temporally and neovascularization of the disc in the left eye (Figure 2).
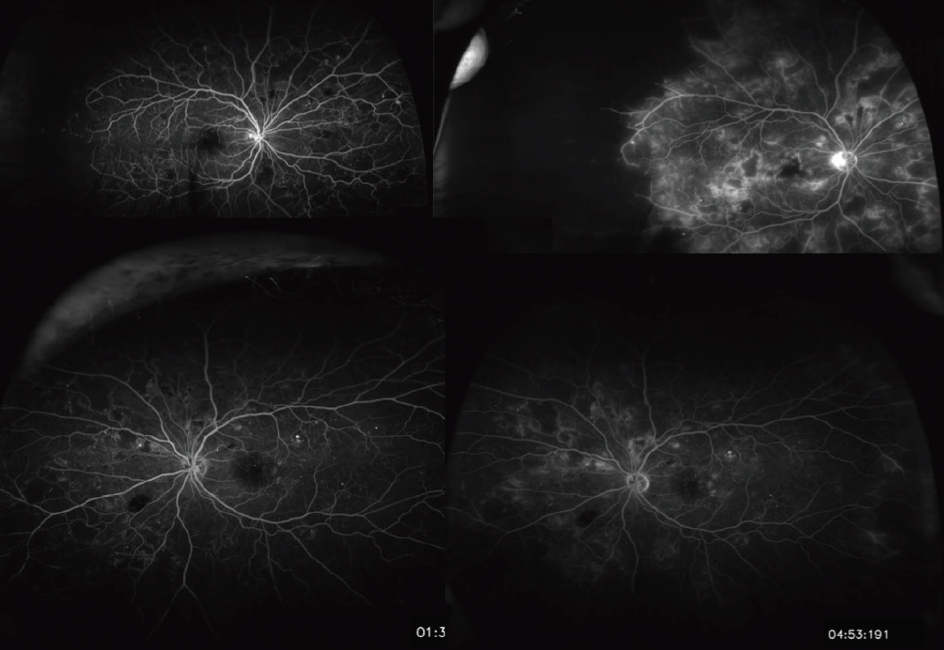
Figure 2. The results of fluorescein angiogram performed on the patient during the initial evaluation.
Case Discussion
Rishi P. Singh, MD: How would you treat the neovascular glaucoma in a patient like this? Is there concern that an anti-VEGF agent might raise the pressure, even transiently? Does the fact that he is reporting eye pain and is symptomatic from the neovascular glaucoma sway your decision?
Nikolas J.S. London, MD: I would tend to be pretty aggressive in a case like this. I would start anti-VEGF injections and consider decompressing prior to the injection or doing an anterior chamber tap afterward.
Tarek S. Hassan, MD: I would do the same.
Nancy Holekamp, MD: If I were concerned about the pressure in a patient like this, I would give only half the dose and would follow with laser within a week.
Dr. Singh: To add to this case, the patient is employed by an auto manufacturer, and he is responsible for operating a piece of machinery on an assembly line. He is routinely monitored with dilated fundus examination and visual fields as a requirement for his job, and if he loses any part of his vision, he cannot perform his work duties. However, he relayed that he was told previously that he had no retinopathy, so the value of those exams is suspect. Nevertheless, my preference is not to do panretinal photocoagulation on the same day as the initial visit unless the presentation really demands it. And so, a decision was made to start IOP-lowering medications and perform an anterior chamber tap, followed by anti-VEGF injections in each eye. I scheduled him for possible laser treatment within 6 or 7 days after this and a pressure check.
Dr. Holekamp: I would want to see a visual field test performed as soon as he was stabilized to establish a baseline.
Dr. London: I would be concerned about the level of compliance in a patient with neovascular glaucoma.
Conclusion
After a series of three anti-VEGF injections over a 3-month period, the hemorrhage improved significantly (Figures 3 and 4). Some de novo areas of ischemia were now evident, and there were ghost vessels in the periphery, more pronounced in the right eye. The patient continued on anti-VEGF injections every 2 months, and I eventually started a treat-and-extend protocol using photographs to guide the need for treatment.
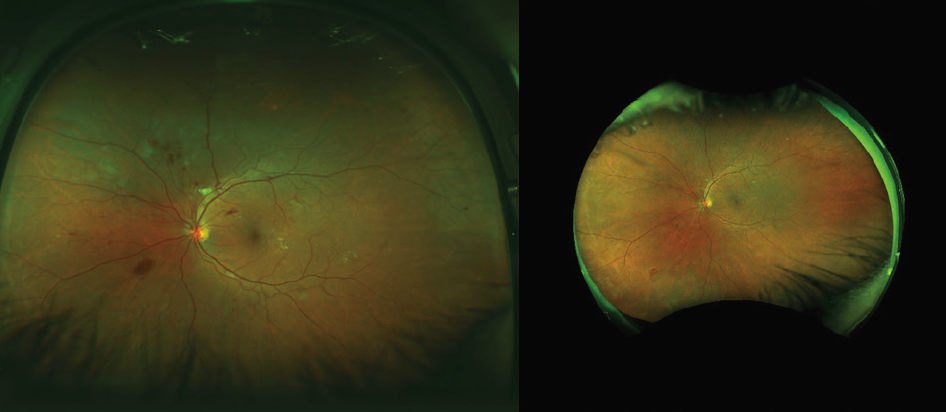
Figure 3. Right eye after three monthly anti-VEGF injections (presentation on the left side and posttreatment on the right side).
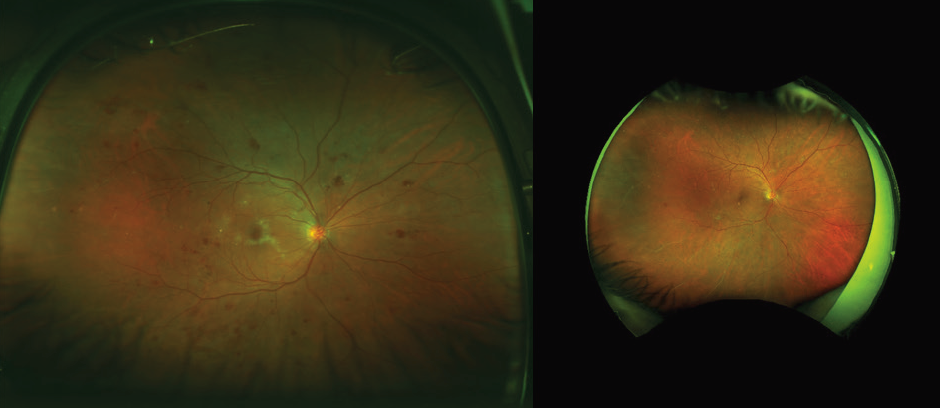
Figure 4. Left eye of the same patient after three monthly anti-VEGF injections (presentation on the left side and posttreatment on the right side).
We are now performing bilateral injections every 3 months in this patient, and the eye is now stable, albeit with a slightly compromised visual field.
For me, this case demonstrates some of the realities of treating diabetic retinopathy in working patients and the urgent need to help preserve vision.