Case Background
- A case of 67-year-old woman with a 15-year history of diabetes who was referred by her ophthalmologist for evaluation of bilateral proliferative diabetic retinopathy.
- The eye was largely asymptomatic, and the patient stated that she was unsure of why she was sent to my clinic.
- VA was 20/40 OD and 20/30 OS at the time of examination, and her hemoglobin A1C level was 6.8.
- On examination, some areas of neovascularization were evident, more pronounced in the right eye, and there was mild diabetic macular edema (DME) in each eye (Figure 1).
- There were areas of nonperfusion in each eye, more so in the right eye.
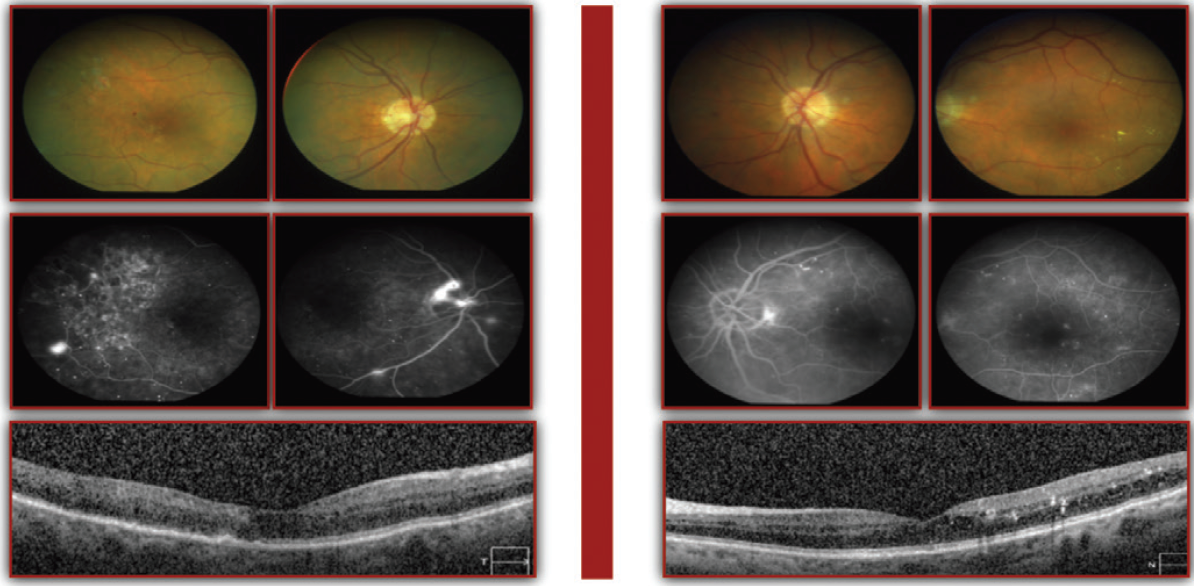
Figure 1. Despite signs of bilateral proliferative diabetic retinopathy, this patient was 20/40 OD and 20/30 OS at the time of presentation and was otherwise asymptomatic.
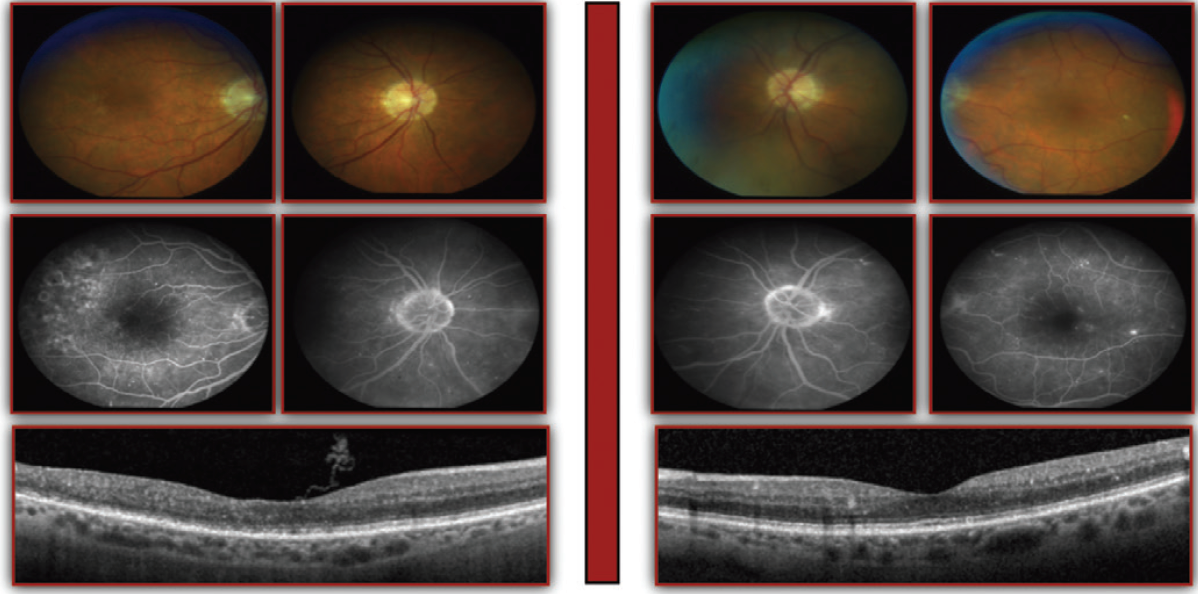
Figure 2. Decreased DME compared to baseline is evident after three anti-VEGF injections. The neovascularization also regressed.
Treatment Plan
- In the past, this is a patient we likely would have observed off therapy based on the presentation of mild DME.
- Other treatment options might have included panretinal photocoagulation or focal laser for the right eye.
- After discussing the options with the patient, a decision was made to start anti-VEGF injections in each eye.
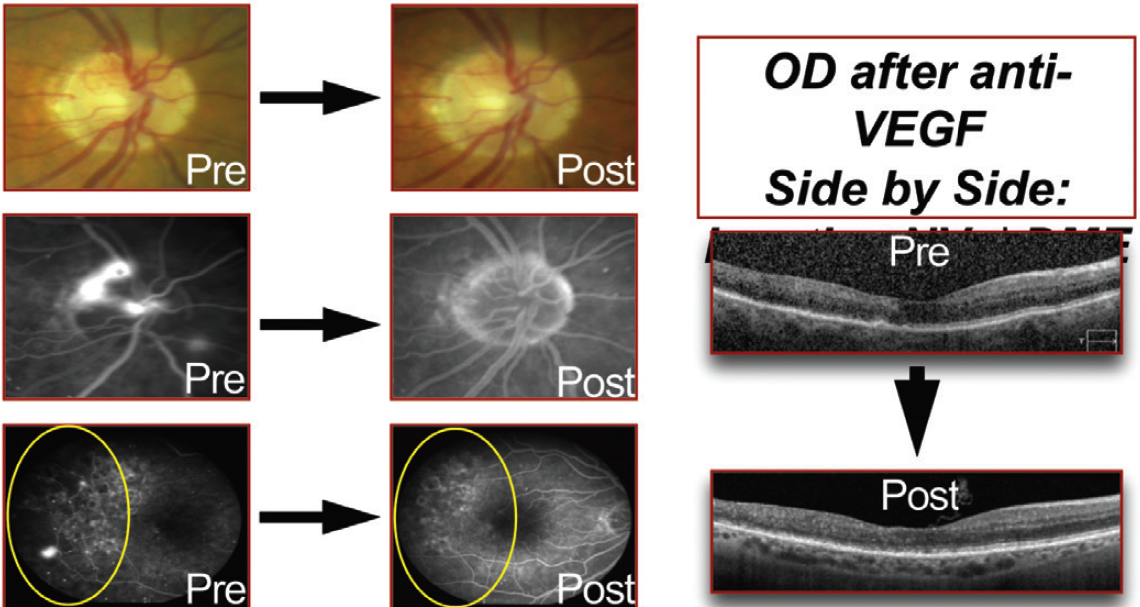
Figure 3. Pre- and posttreatment comparisons.
Case Discussion
Nancy Holekamp, MD: It is evident that treatment options have expanded. Even with respect to anti-VEGF injections, it would have been reasonable to inject just in the left eye and observe the right eye. More options for treatment might mean that our conversations with patients are longer and more involved, but the expanded options really make that a worthwhile discussion.
Tarek S. Hassan, MD: After three ranibizumab (Lucentis, Genentech) injections, the neovascularization regressed in both eyes, and the mild DME resolved in each eye (Figure 2). VA improved to 20/25 in each eye, which represented a 2-line gain in Snellen acuity. The effect of anti-VEGF injections on the status of the retina is easily apparent on color fundus photographs and fluorescein angiography (FA) after only three monthly ranibizumab injections (Figure 3).
Arshad M. Khanani, MD, MA: What did you do long-term with this patient?
Dr. Hassan: Anti-VEGF injections have been continued, and I more than likely will start a treat-and-extend protocol, hopefully extending to every 3 to 4 months.
Nikolas J.S. London, MD: Will you repeat FA each time, looking for redevelopment of neovascularization to determine the interval?
Dr. Hassan: I will monitor for that. In general, I increase the interval by 1 to 2 weeks at a time, hopefully extending to several months. I do not repeat FA to look for neovascularization. That is something I look for clinically and then follow up with OCT to monitor for DME. I may occasionally obtain FA to assess my progress in controlling the neovascularization, but certainly this is not something that is needed frequently.
Conclusion
Overall, this patient is very happy with the way treatment is unfolding. This case demonstrated that we can introduce anti-VEGF therapy, even for patients in whom we typically might not think about using it, because of our ability to prevent progression of the overall disease. Observation would have been a reasonable approach, and in fairness, there might not have been any progression in the short term. But here, we are being proactive rather than reactive in managing this patient’s disease, which is an important shift in how we treat diabetic retinopathy.
