Microincisional vitrectomy has become the standard for the management of complex diabetic tractional retinal detachments (TRDs). The vitrectomy cutter is typically used to access the space between the adherent hyaloid and fibrovascular membranes. In some cases, however, additional maneuvers are needed to safely and successfully remove the membranes.
Multiple techniques and tools have been described for membrane dissection, including forceps, scissors, pics, viscodelamination, and bimanual techniques.1,2 In 2003, Fortun and Hubbard reported on the use of a new viscodissector designed for small-gauge vitrectomy (25-gauge and smaller), with automated injection of the viscoelastic and an extendable tip for ease of use and access into the surgical planes.3
The use of digital video recording with 3D capabilities in ophthalmic surgery is being adopted rapidly by vitreoretinal surgeons.4 The video recording consists of a dual high dynamic range 4K camera that captures the images from each ocular of the microscope and displays them on a 4K ultra high-definition monitor. The surgeon wears 3D eyeglasses to visualize the surgical images on the heads-up display. Multiple reports have shown that 3D heads-up display provides benefits over the traditional microscope in vitreoretinal surgery as it can improve posture, enhance the depth of field, increase image size, and improve image quality through digital manipulation.4
In this case, we present the use of the viscodissector and the 3D heads-up display to manage a complex diabetic TRD.
Case Presentation
A 39-year-old female with a history of type 1 diabetes mellitus presented with progressive vision loss in both eyes with recent worsening of vision loss in the right eye. The initial examination showed VA of 20/1000 in the right eye and 20/125 in the left eye. Dilated fundus examination revealed active proliferative diabetic retinopathy with combined tractional and rhegmatogenous retinal detachment of both eyes (Figure 1). Preoperative anti-VEGF injection was administered with subsequent repair of the complex retinal detachment of the right eye.
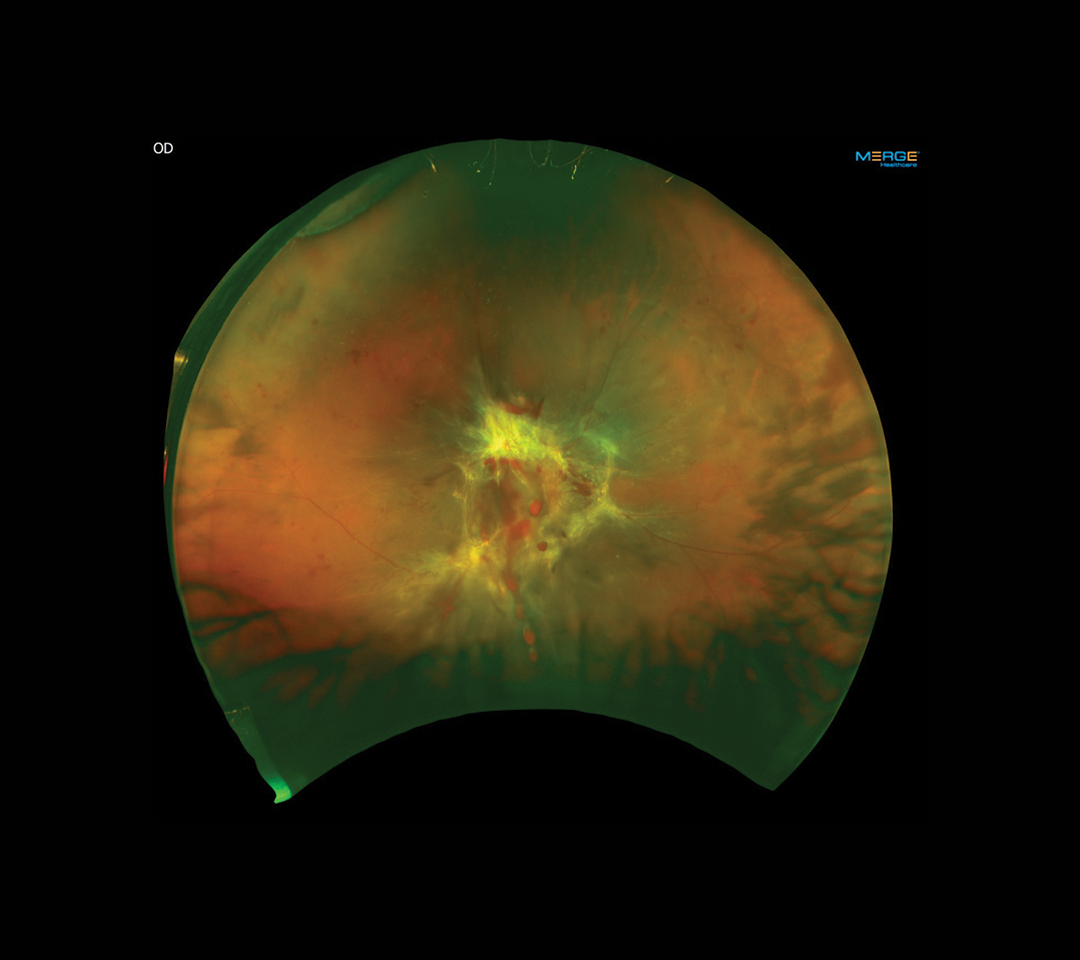
Figure 1. The patient’s right eye shows active proliferative diabetic retinopathy with combined tractional and rhegmatogenous retinal detachment.
This case was performed using the NGENUITY 3D Visualization System (Alcon) and the CONSTELLATION Vision System (Alcon) with 25-gauge instrumentation. A standard three-port pars plana vitrectomy was performed. Upon examination of the retina intraoperatively, it was determined that the membranes were extensive and that the broad adhesions were ideal for removal with viscodissection. After core vitrectomy was performed, the antero-posterior vitreous traction was released for 360º.
The 3D heads-up display provided enhanced depth perception and increased image size, which facilitated visualization of the surgical planes for successful membrane removal. The 25-gauge vitrector was chosen, as this small gauge allows for easier access and manipulation of the space between the membranes and the retina. The posterior hyaloid was entered with the vitrector, the Hubbard viscodissector (Bausch + Lomb) was placed through the opening of the hyaloid, and a combination of mechanical and viscoelastic delamination was performed with subsequent cutter segmentation and membrane removal.3 A small retinal hole was noted, and this was used to drain subretinal fluid followed by laser. Silicone oil was used for retina tamponade.
The patient did very well with improved VA and stable retina. Subsequent silicone oil removal with cataract extraction was performed, and the patient achieved 20/70 VA 1 year after the initial surgery (Figures 2 and 3).
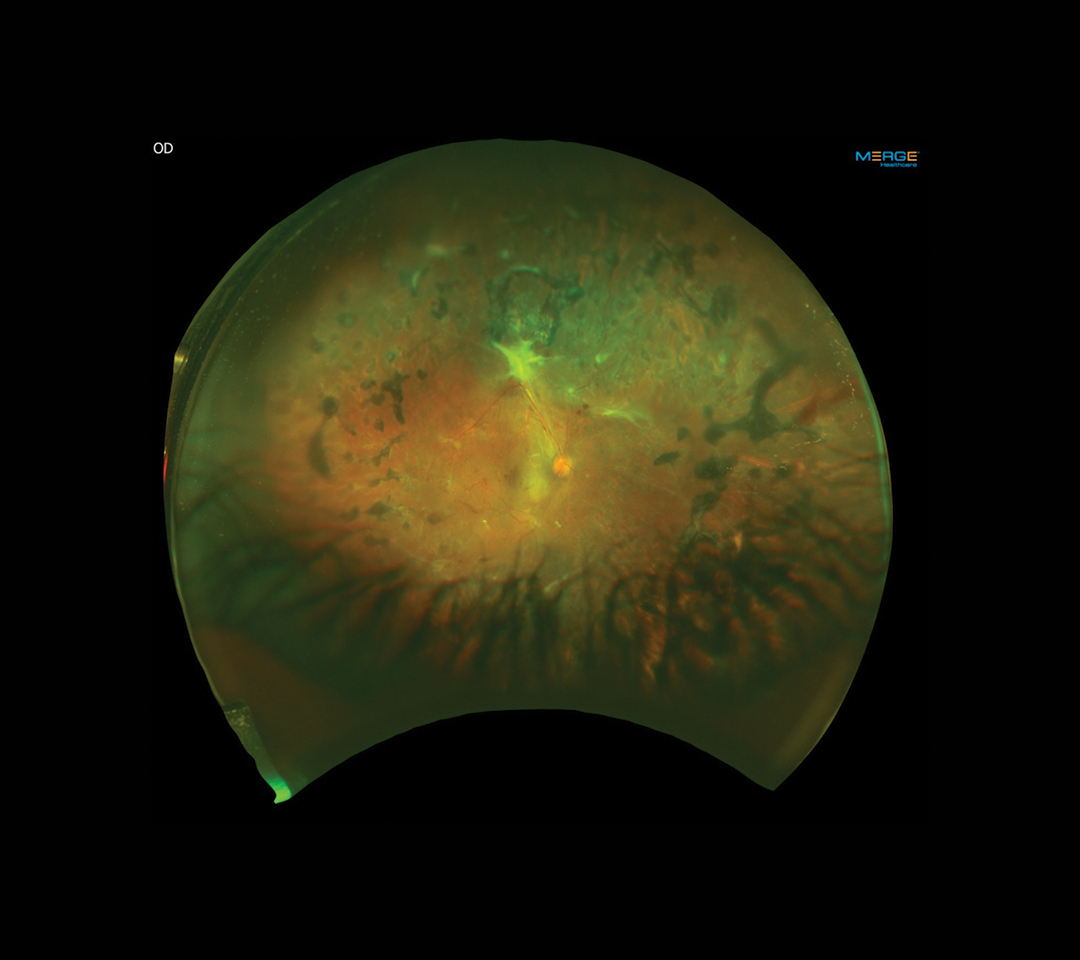
Figure 2. Postoperative fundus photo 1 year after surgery showing attached retina with peripheral panretinal photocoagulation.
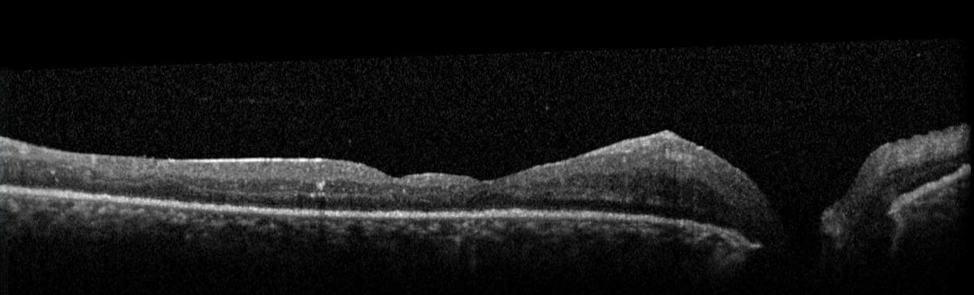
Figure 3. Postoperative OCT showing attached retina after membrane peel.
Discussion/Conclusion
The use of a 3D heads-up display in this complex TRD case provided enhanced depth of field and visualization of the membranes and surgical planes, which facilitated membrane identification and dissection.
The broad adhesions between the diabetic fibrovascular membranes and the retina in this case were ideal for the use of the Hubbard viscodissector, which allowed safe and successful delamination of the membranes with subsequent segmentation and removal. Our video demonstrates that this instrument is effective and safe to use in the management of these complex diabetic cases, particularly when used with the heads-up 3D surgical display (Video).
Luis J. Haddock, MD; and Jorge Fortun, MD, present a case of viscodissection in a diabetic tractional retinal detachment (TRD) using Alcon’s NGENUITY 3D Visualization System with heads-up display.
1. Sharma S, Hariprasad SM, Mahmoud TH. Surgical management of proliferative diabetic retinopathy. Ophthalmic Surg Lasers Imaging Retina. 2014;45:188-193.
2. McLeod D, James CR. Viscodelamination at the vitreoretinal juncture in severe diabetic eye disease. Br J Ophthalmol. 1988;72:413-419.
3. Fortun JA, Hubbard GB 3rd. New viscodissection instrument for use with microincisional vitrectomy in the treatment of diabetic tractional retinal detachments. Arch Ophthalmol. 2011;129:352-355.
4. Eckardt C, Paulo EB. Heads-up surgery for vitreoretinal procedures: an experimental and clinical study. Retina. 2016;36:137-147.