Retinal fold formation is a rare but potential complication following rhegmatogenous retinal detachment (RRD) repair via scleral buckling (SB), pars plana vitrectomy (PPV), or pneumatic retinopexy with internal gas tamponade.1 These folds may result in decreased VA and significant metamorphopsia when present in the macula.1 In canine studies, extensive loss of photoreceptors has been demonstrated within retinal folds.2
The basic pathophysiology of fold formation involves the inadvertent compression and trapping of stretched, redundant neurosensory retina during retinal reattachment.3 Risk factors include bullous superior retinal detachment (RD) (particularly macula splitting), recent onset of detachment (low viscosity of subretinal fluid may rapidly resorb and result in irregular reattachment), high circumferential SBs (increased retinal redundancy), and RD running through the fovea.3 In addition, the use of intraocular gas tamponade combined with scleral buckling surgery may push fluid posteriorly, resulting in folding when the retina attempts to reattach to a reduced internal eye-wall circumference.4
Traditional indications to reoperate include the presence of full-thickness folds involving macula and epiretinal membrane (ERM)-induced macular traction/folds. Traditional indications to observe include partial-thickness macular folds and extramacular folds.5
The following cases highlight a variety of retinal folds and the various strategies employed to manage them. We also suggest that the presence of foveal ectopia may be another clinical sign guiding treatment.
Foveal Ectopia
Foveal ectopia has been described in the literature and is defined in the postoperative context as a deviation of the position of the fovea centralis with respect to the optic nerve head relative to the preoperative position.6 Near-infrared (NIR) imaging accompanying the spectral-domain OCT image can be used to compare pre- and postoperative images to identify foveal ectopia. If preoperative imaging is unavailable, the postoperative deviation relative to the other eye can be used as a surrogate to assess for this parameter.6
Case 1: Full-Thickness Macular Fold
A 66-year-old female who is pseudophakic was treated with PPV and insertion of 12% C3F8 internal gas tamponade for a macula-off bullous superior RD. At postoperative week 3, the patient noted continued poor vision of counting fingers and a “large line” in the center of her vision. Of note, the patient developed choroidal detachments on postoperative day 1, with a normal IOP. A full-thickness macula-splitting retinal fold was present (Figure 1A). There was no foveal ectopia.
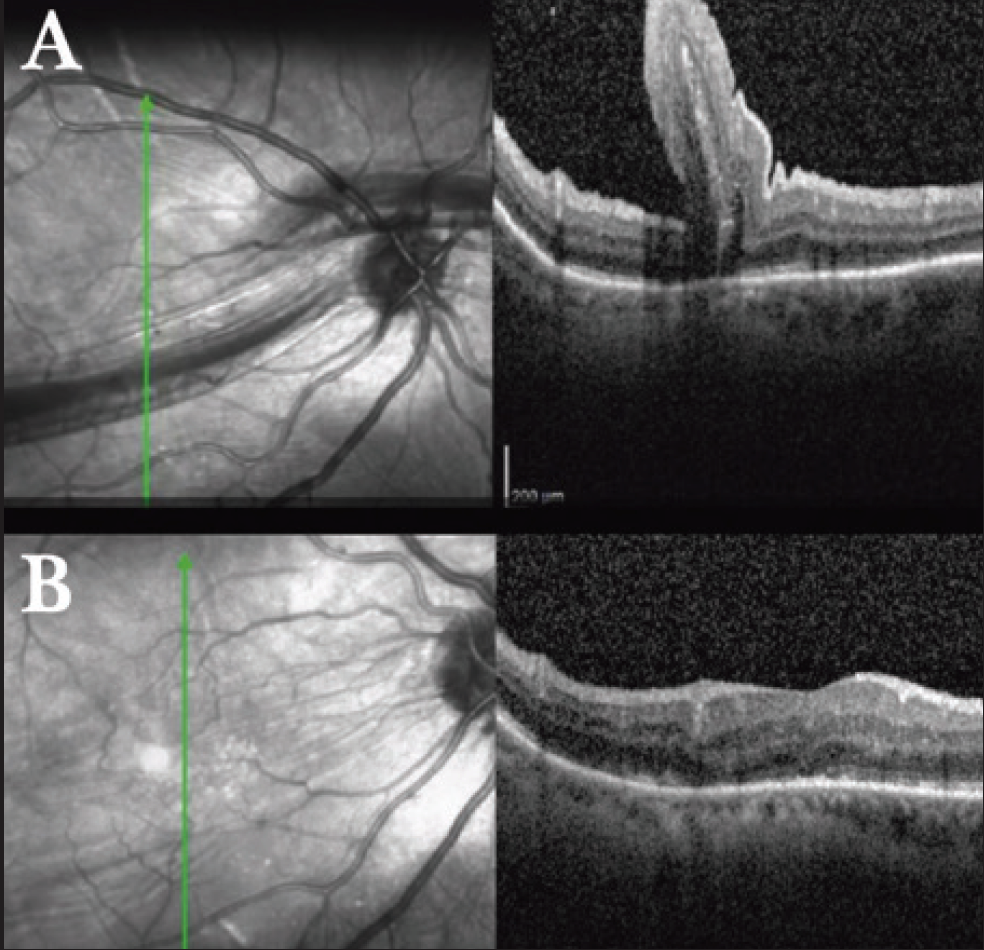
Figure 1. Case 1: NIR and OCT imaging 3 weeks after RD repair (A). After macular redetachment, postoperative month 3 imaging demonstrates resolution of the fold and foveal ellipsoid zone loss (B). VA was 20/100 with resolution of the linear scotoma.
The patient was returned to the OR where macular detachment was induced using balanced salt solution in multiple locations using a 41-gauge cannula (De Juan/Awh, Synergetics). The retinal fold was manually separated using a diamond-dusted membrane scraper (DDMS, Synergetics). Perfluorocarbon liquid (Perfluoron, Alcon) was used to flatten and stabilize the posterior retina. Subsequently, a fluid-air exchange was performed, and the subretinal fluid was drained through a peripheral retinotomy.
At postoperative month 3, VA was 20/100, and OCT showed successful resolution of the macular fold with some ellipsoid zone loss at the fovea (Figure 1B). The patient reported improved vision, no distortion, and resolution of the linear scotoma (Video).
Larry Puthenparambil, MD, performs a manual macular retinal fold repair using a diamond-dusted membrane scraper (DDMS, Synergetics), followed by the use of perfluorocarbon liquid (Perfluoron, Alcon), fluid-air exchange, and subretinal fluid drainage on a pseudophakic patient who noted continued poor vision of counting fingers and a “large line” in the center of her vision on postoperative week 3 following surgery.
Case 2: PVR ERM With Underlying Macular Fold and Foveal Ectopia
A 49-year-old-male (born prematurely) presented with 2.5 weeks of superior RD with immature proliferative vitreoretinopathy (PVR). The patient was hospitalized at that time after undergoing a below-the-knee amputation due to chronic foot pain.
The patient initially underwent SB, PPV, membrane peeling, and 14% C3F8. An incomplete posterior vitreous detachment was noted, and meticulous attention was taken to use triamcinolone (Kenalog, Bristol-Myers Squibb) to stain the posterior hyaloid and ensure complete removal. The immature PVR was scraped with a flex-loop (Finesse, Alcon), but there were no definitive membranes to peel. ILM peeling was not performed.
Postoperatively, the patient struggled to maintain face-down positioning because of his recent below-the-knee amputation; he was frequently on his back. His vision 10 weeks postoperatively was hand motions with a dense posterior subcapsular cataract and no view of the posterior pole.
After successful cataract surgery and IOL placement, a dense PVR ERM with inferior macular dragging (foveal ectopia) and underlying retinal fold (Figure 2A) was noted. The patient underwent PPV with membrane peeling. The macular fold was partial thickness after removal of the ERM; thus macular detachment to unfurl the fold was not attempted.
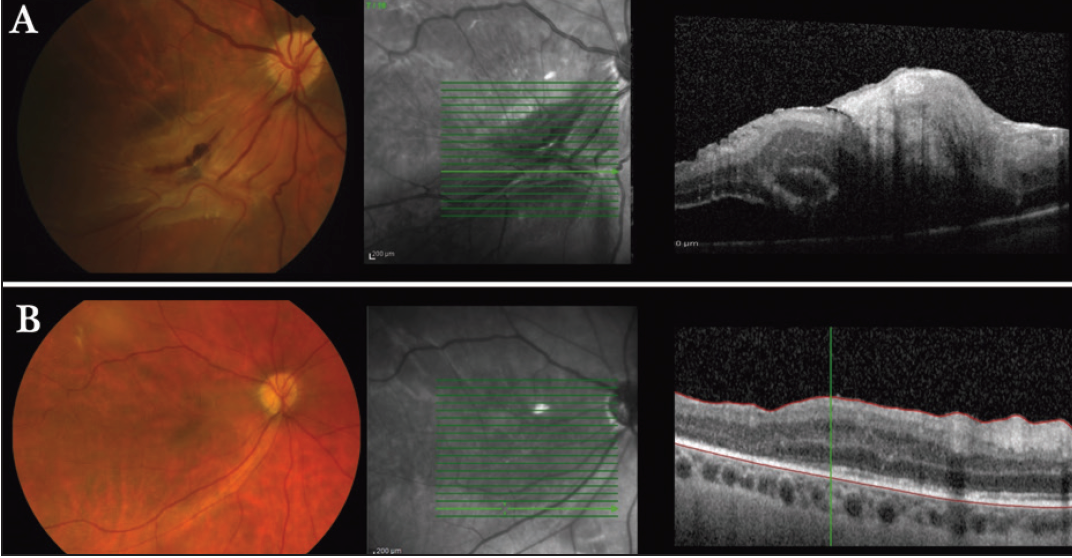
Figure 2. Case 2: multimodal imaging after primary SB and vitrectomy to repair a RD (A). PVR/ERM-induced inferior macular dragging with underlying retinal folding evident on color photography, NIR, and OCT. After PPV with ERM and ILM peeling, VA improved to 20/100, but metamorphopsia persisted (B). Despite resolution of the macular folds on OCT, inferior foveal dragging is evident on color photography and NIR imaging.
Postoperatively, the ERM resolved, but significant inferior foveal ectopia remained, and the patient had symptomatic blurry vision with BCVA 20/100 and image distortion (Figure 2B).
Case 3: Extramacular Fold With Foveal Ectopia
A 61-year-old phakic male had a bullous macula-detached superior RD of 7 days’ duration and underwent SB/PPV/20% SF6 surgery. A full-thickness inferior extramacular fold with inferior foveal ectopia was seen on examination postoperatively (Figure 3A). Foveal ectopia was confirmed on NIR imaging. VA was 20/200, and the patient reported significant binocular diplopia with a torsional component and metamorphopsia.
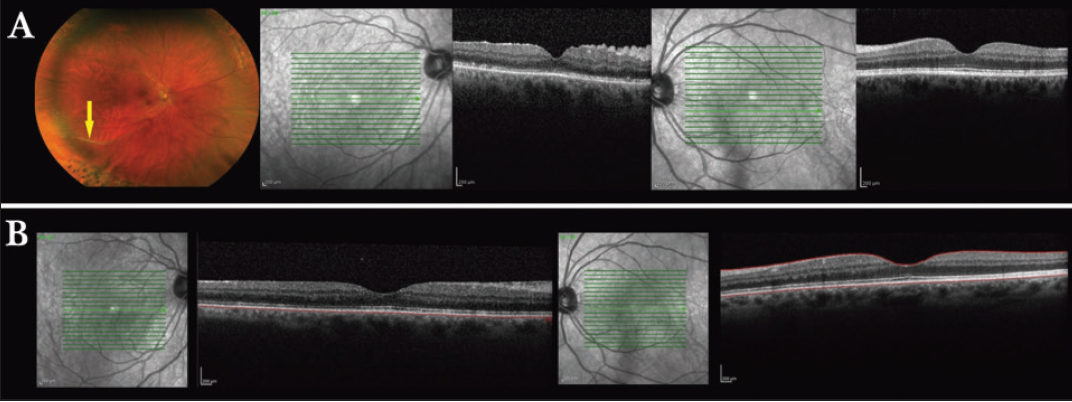
Figure 3. Case 3: multimodal imaging 7 days after repair of a bullous macula-off superior RD (A). A full-thickness extramacular fold of the right eye with foveal dragging was seen on color fundus photography (yellow arrow). Comparison of NIR images from the affected and unaffected eye demonstrates inferior foveal placement of the right eye relative to the left eye. Observation for the retinal fold was recommended, and at postoperative month 9, the fold had resolved (image not shown). Repeat comparison of NIR images from the two eyes reveals persistent foveal ectopia (B). The patient experienced metamorphopsia. VA in the affected eye was 20/30.
The retinal fold was attributable to incomplete subretinal fluid evacuation at the time of surgery with improper positioning. The binocular diplopia was believed to be related to the SB. Observation was recommended for the retinal fold, given its extramacular location; however, removal of the SB was performed to address the binocular diplopia.
By postoperative month 9, the fold had resolved, and VA was 20/30. The binocular diplopia was partially alleviated with oblique prism correction; however, foveal ectopia persisted relative to the contralateral eye (Figure 3B), and debilitating complaints of metamorphopsia remained.
Discussion
Retinal folds have a broad variety of presentations, management, and outcomes, as is evidenced by these cases. Case 1 presented with a full-thickness macular fold with improvement of metamorphopsia but VA compromise owing to photoreceptor loss. Case 2 demonstrates that, despite surgical intervention to alleviate the tangential traction from a macular PVR membrane, there was significant retinal dragging with inferior foveal ectopia and image distortion. Similarly, in case 3, despite great final VA and spontaneous resolution of an extramacular fold, foveal ectopia was associated with persistent complaints of monocular distortion.
Pearls to Minimize Retinal Folds After Routine RRD Repair
- Have a high threshold to minimize folds in cases that are at high risk of developing a macular fold, such as superior macula-splitting detachments.
- Minimize the amount of posterior fluid in cases at high risk for developing postoperative macular fold.
- Employ measures—such as enlarging small breaks, utilizing perfluorocarbon or a posterior retinotomy, and performing a slow and complete fluid-air exchange.
- Minimize the risk of fold formation in cases with significant posterior fluid at the conclusion of RRD repair by utilizing proper face-down positioning immediately postoperatively (or temporal side down in patients who cannot face down).
In comparing the first case to the second two, the consideration of foveal ectopia appears relevant. Further research is needed to determine if foveal ectopia in the immediate postoperative course warrants surgical intervention with macular redetachment with the goal of restoring retinal anatomy to a more physiologic location.
Conclusion
Retinal folds are rare and potentially severe complications of RRD repair. We have noted that foveal ectopia may be a potential indicator of poor outcome, regardless of final BCVA. Future studies should consider this parameter to better understand how significant the variable is in determining final outcome.
1. Larrison WI, Frederick AR Jr, Peterson TJ, Topping TM. Posterior retinal folds following vitreoretinal surgery. Arch Ophthalmol. 1993;111:621-625.
2. Hayashi H, Yamashiro K, Tsujikawa A, Ota M, Otani A, Yoshimura N. Association between foveal photoreceptor integrity and visual outcome in neovascular age-related macular degeneration. Am J Ophthalmol. 2009;148:83-89.
3. Heimann H, Bopp S. Retinal folds following retinal detachment surgery. Ophthalmologica. 2011;226 Suppl 1:18-26.
4. Lewen RM, Lyon CE, Diamond JG. Scleral buckling with intraocular air injection complicated by arcuate retinal folds. Arch Ophthalmol. 1987;105:1212-1214.
5. Ahn SJ, Woo SJ, Ahn J, Park KH. Spontaneous resolution of macular fold following retinal reattachment: morphologic features on SD-OCT. Ophthalmic Surg Lasers Imaging. 2011;42 Online:e81-83.
6. Williams TD, Wilkinson JM. Position of the fovea centralis with respect to the optic nerve head. Optom Vis Sci. 1992;69:369-377.




