Patient History
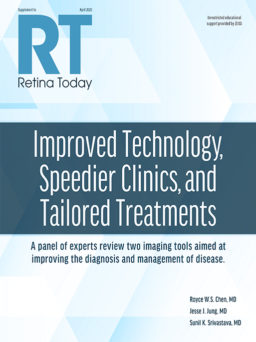
- Patient with bilateral AMD; OCT of the left eye showed large pigment epithelial detachment (PED) and presence of intraretinal (IRF) and subretinal fluid (SRF). Central subfield thickness (CST) was 348 µm (Figure 1)
- Right eye had intermediate AMD at this stage (not shown)
- VA was 20/100
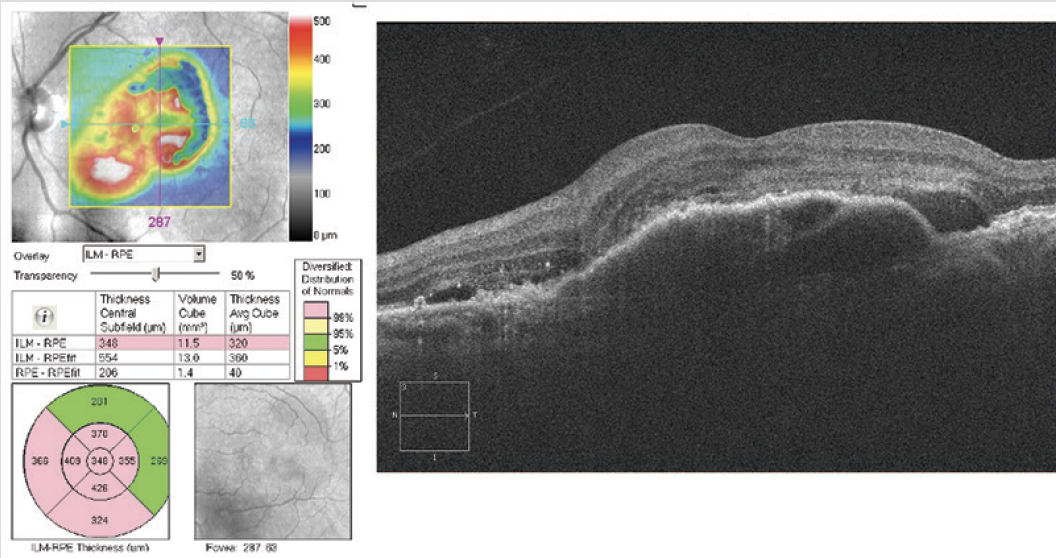
Figure 1. Left eye of a patient with bilateral AMD (OS>OD).
Intervention
- The patient was started on anti-VEGF therapy, and after 5 injections over 6 months, CST improved, although some accumulation of subretinal hyperreflective material was present (not shown)
- After 1 year and 11 total injections, VA in the left eye was 20/25 with resolution of IRF and SRF (Figure 2a); however, the right eye now started to show shallow PEDs and evidence of SRF (Figure 2b)

Figure 2. After 1 year, the right eye started to show early signs of AMD progression (A, left) while monthly treatments have achieved some control in the left eye (B, right).
Discussion
Rishi P. Singh, MD: The left eye has required a high-injection frequency and is still not dry, even with treatment every 5 weeks. Is there anything you might do differently in the left eye to improve this anymore?
Carl D. Regillo, MD: You are already at 20/25 vision. I think that looks quite nice. You have had a nice improvement. I’m a little worried about some early fibrosis that could affect visual outcomes over time. I’m also a little concerned now about the right eye showing signs of exudation, so I’d be inclined to start treating that eye sometime soon.
Caroline R. Baumal, MD: In the left eye, there’s probably choroidal neovascularization. There’s some sort of outer retinal hyperreflectivity. Are those cysts? Are those active? Is there formation of outer retinal tubulations over the fibrosis? Time will tell in the left eye. I might try to extend it a bit. But I would not want to lose the gains in the left eye if the vision is good. In the right eye, under the PED, there’s probably some neovascularization. I find that eyes like that can be very difficult to treat sometimes. I would treat that right eye. It looks active to me.
Dr. Singh: Two years later, VA is 20/30 in the left eye after 16 anti-VEGF injections. The vision has been maintained despite having some IRF and subretinal hyperreflective material (not shown). In the right eye, no additional fluid, but the PED collapsed, and there are now transmissional defects present. The patient manifests a small submacular hemorrhage. By 3 years from the initial visit, the left eye has received 20 total injections and is being treated with a fixed interval between 8 and 10 weeks; the right eye has received 11 injections. The right eye has fully converted (Figure 3). How do you approach treatment at this point?

Figure 3. After 2 years, the right eye (A, left) has converted to neovascular AMD while consistent treatment of the left eye (B, right) has achieved control.
Dr. Regillo: I would treat both eyes at this visit, have the patient come back in a month, and treat the right eye until all signs of exudation are gone on a monthly basis. Then I would work to extend that eye such that it matches up with the left. That should not take too many visits if you’re treating the left eye relatively frequently. The right eye, because it’s caught a bit earlier, you might even be more successful in not only achieving a good vision outcome, but in extending the interval even more.
Dr. Singh: Through 4 years, the patient received 12 injections OD and 22 injections OS and VA was 20/30 OD and 20/100 OS. By a full 5 years from the initial visit, we had taken our foot off the gas a little bit: 13 total injections OD (VA 20/30) and 24 total injections OS (VA 20/70). There was recurrence of both IRF and SRF (Figure 4). A graph of CST over time in this patient extracted from our EMR system showed variability in CST, which may be a negative prognosticator for final visual outcome (Figure 5).
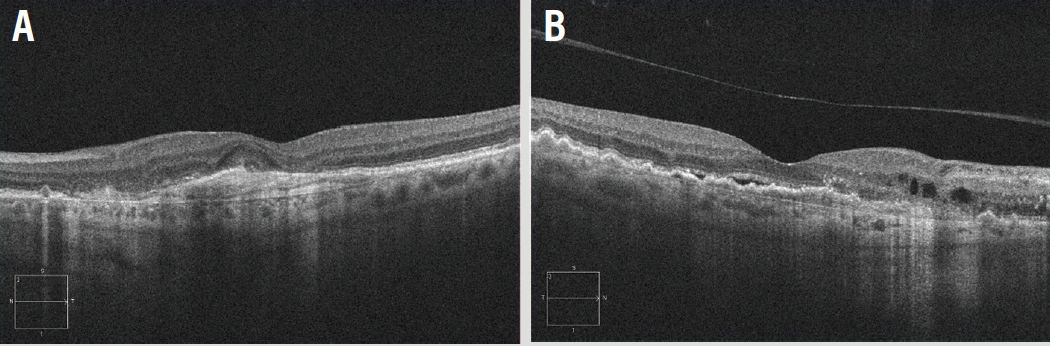
Figure 4. Extending the intervals too much between years 4 and 5 proved problematic for the outcome.

Figure 5. A graphical representation of CST variability over time available through our Image management system (Zeiss Forum Retina Workplace) has become a useful tool for evaluating long-term visual prognosis.