The incidence of ROP has increased in recent years as a result of advances in neonatal care and the subsequent increase in premature births.2,3,21 In 2010, ROP was the cause of severe visual impairment or blindness in 1.1% of children in high-income countries (defined by the World Bank as those with a gross national income per capita of US$12,376 or more in 2018) and 2.5 to 2.8% of children in other regions (including middle- and low- income countries in Eastern Europe, Central Asia, Latin America, and Africa).22
In middle-income countries, due to differences in standards of care in neonatal intensive care units (NICUs) compared with high-income countries, use of the same screening standards implemented in high-income countries may not be appropriate.23 “In a study carried out in our hospital, we discovered that 100 of 352 newborns with ROP evaluated between January 2011 and March 2017—nearly one-third—fell outside the current screening guidelines of the American Academy of Ophthalmology, having a birth weight greater than 1,500 g or a gestational age of more than 30 weeks,23” said Prof. Maria Ana Martinez-Castellanos.
The pathophysiology of ROP is characterized by abnormal neovascularization. The disruption of angiogenesis in preterm infants with ROP typically occurs in two postnatal phases.24 In phase 1 (from birth up to 30 weeks’ postmenstrual age), hyperoxia inhibits vascular growth in the retina.5 As the retina becomes more metabolically active (from around 30 weeks’ postmenstrual age), its incomplete vascularization causes it to become hypoxic, resulting in the secretion of various angiogenic factors including VEGF and subsequently to VEGF-driven neovascularization and intraocular fibrosis.5 Ultimately this can result in retinal detachment and visual disability.5,24
A key early advance in the management of ROP was the formal classification of ROP terminology in the international classification of ROP in the 1980s.25 “With this classification now used worldwide, we’re all talking the same language, which means that we can act appropriately at each stage of the disease,” said Prof. Martinez-Castellanos. According to international classification of ROP terminology, ROP is categorized according to the zones of the retina in which disease is visible via dilated fundus examination and the severity (or stage) of the disease.26
Zone 1 includes the macula and optic nerve; it forms a circle, the radius of which is twice the distance from the optic nerve to the macula (Figure 4). ROP in Zone 1 is the most likely to progress and become severe. Zone 2 surrounds Zone 1 and extends to the ora serrata on the nasal side.26 ROP found here may progress quickly, although warning signs such as increasing vascular dilation and tortuosity usually predate the threshold by a week or 2. Zone 3 is a crescent area of temporal retina, which rarely shows aggressive disease.27
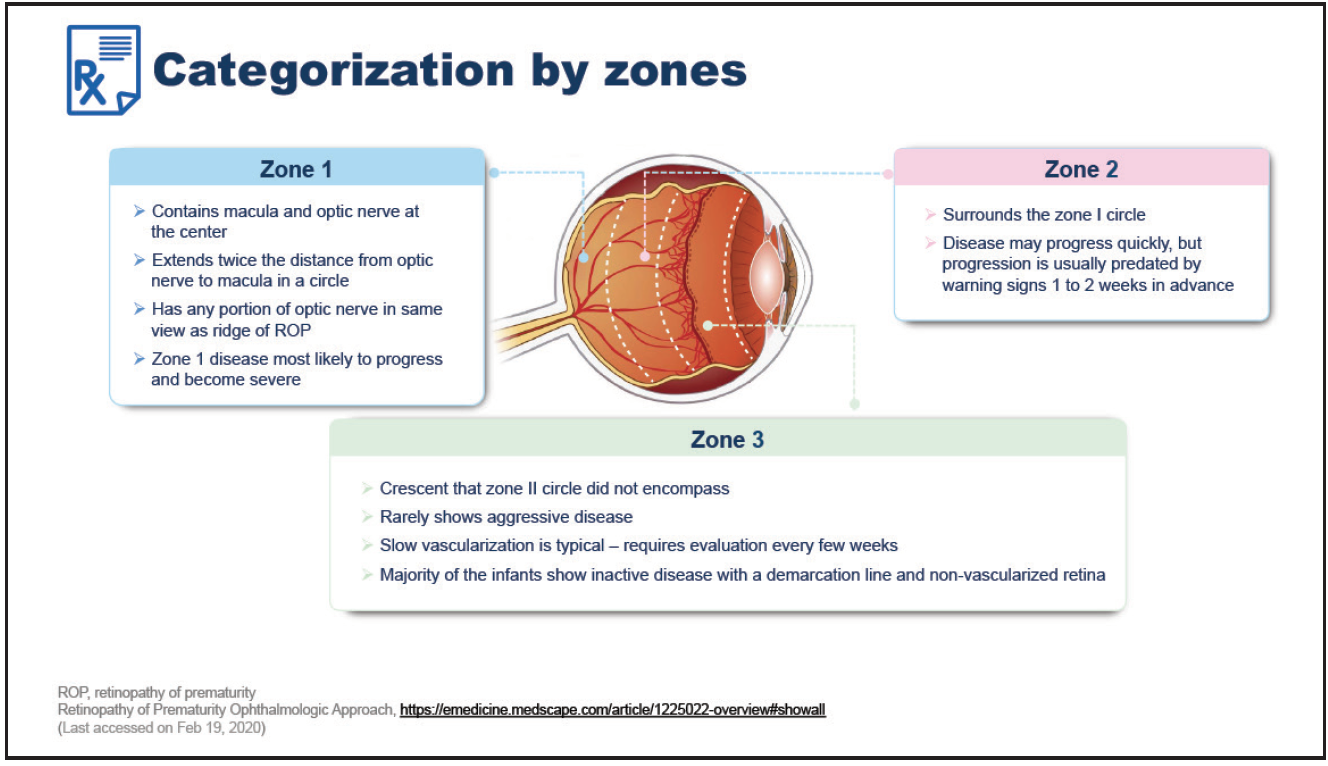
Figure 4. Categorization of ROP by zones.
When categorizing ROP by disease stage, in Stage 1 a demarcation line can be clearly seen between normally vascularized retina and the peripheral retina with no blood vessels (Figure 5).27,28 In Stage 2, the demarcation line is elevated into a ridge, but with no pathological new vessels; in Stage 3 these new vessels are present.27,28 Stage 4 and 5 represent partial and total retinal detachment, respectively.20,21 “Stage 5 is very sad. This means that we are too late to save this eye, and the best outcome following surgery would be only light perception or movement,” said Prof. Martinez-Castellanos. Aggressive posterior ROP (AP-ROP) may also be present. This usually occurs in Zone 1 and can progress very quickly to retinal detachment.27
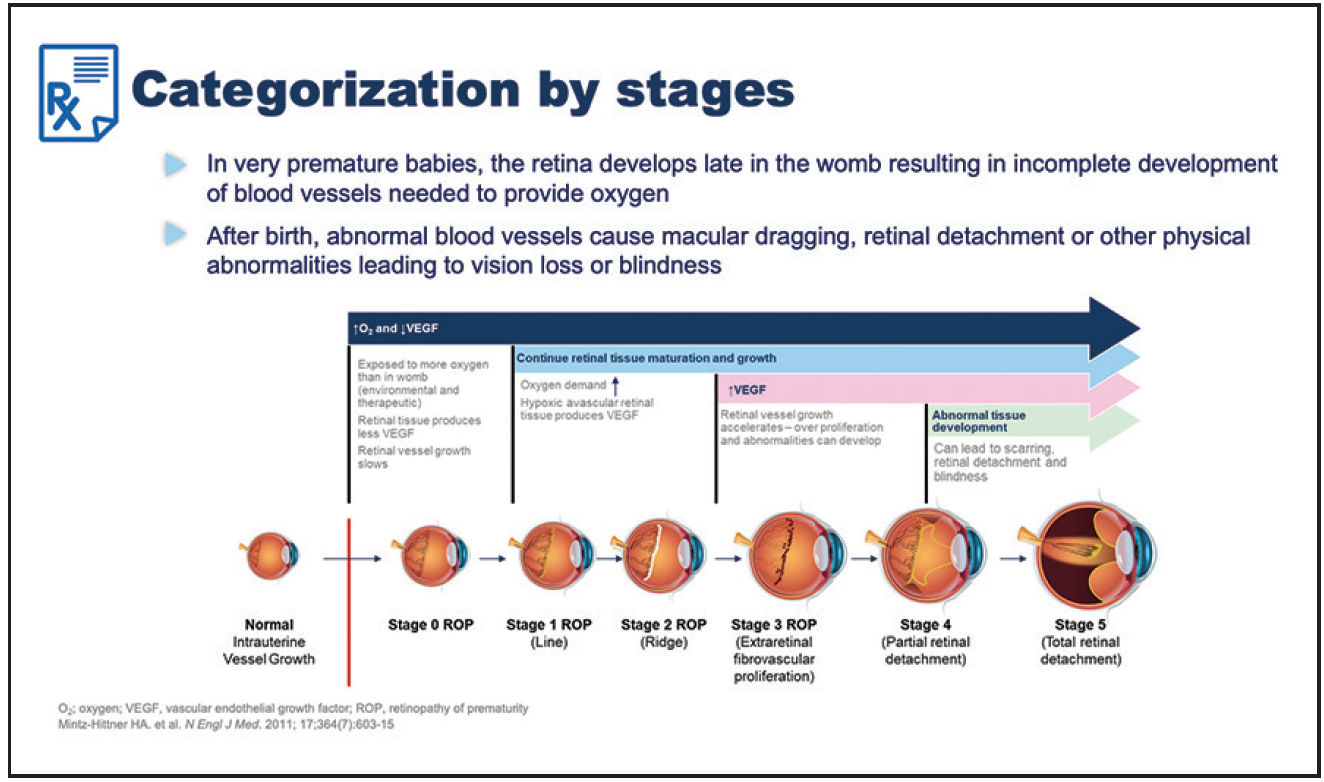
Figure 5. Categorization of ROP by stages.
The zone and stage of ROP can be combined to give the ROP ‘type’ (Figure 6), which differentiates eyes with significant changes of ROP that require treatment (Type 1) from eyes with significant changes that do not require treatment but must be carefully monitored (Type 2).29
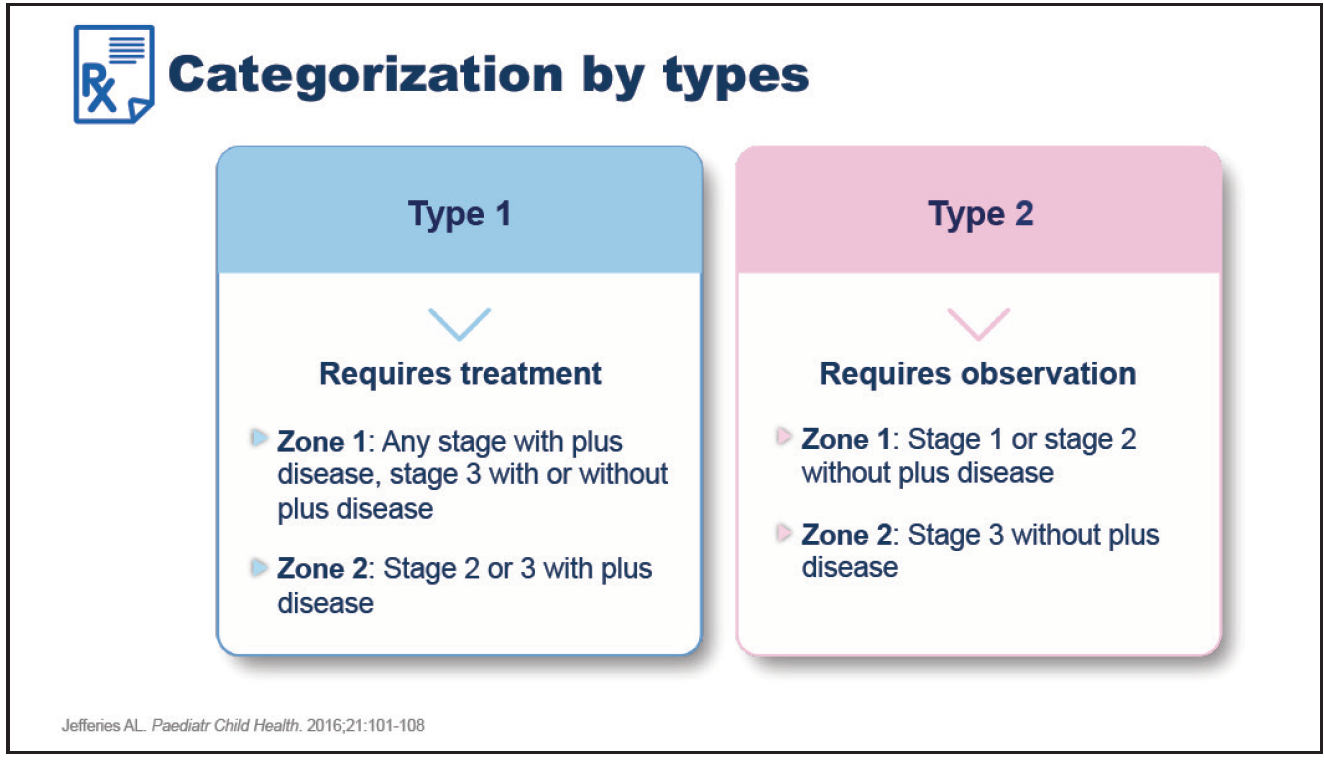
Figure 6. Categorization of ROP by types.
Severe ROP leads to long-term visual loss, with blindness in the most severe cases, so timely treatment is vital.5 ROP is also associated with a range of other eye problems later in life, such as retinal detachment, glaucoma, and refractive errors, so lifelong monitoring is required.5 Traditional treatment options for ROP include cryotherapy and surgery, though these are associated with complications.26 Laser therapy is the current standard of care for treating ROP, but it is an invasive, resource-intensive procedure used in patients with advanced disease only.30 More recently, anti-VEGF therapy is being used for the treatment of ROP, especially in Zone 1.26
Highlights
- Severe retinopathy of prematurity (ROP) leads to long-term visual loss and potential blindness, so timely treatment is vital.
- Lifelong monitoring of ROP is required due to a range of associated eye problems which may occur later in life.
- Traditional treatment options for ROP include cryotherapy and surgery, though these are associated with complications.
- Laser is the current standard of care for ROP, but it is an invasive, resource-intensive procedure used in advanced disease only.
- More recently, anti-VEGF therapy is being used for the treatment of ROP, especially in Zone 1.26
